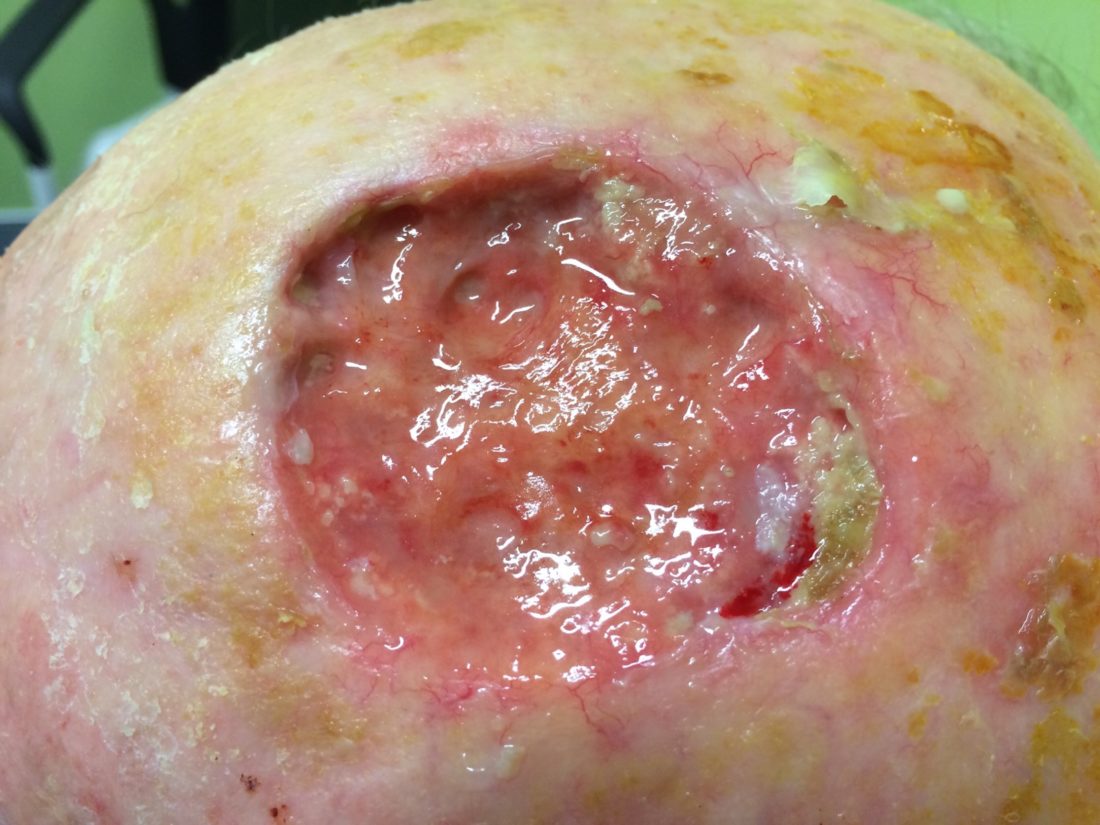
Bringing non-healing wounds into the open
Most clinicians and patients expect their cutaneous wounds to heal – which is fine, until they don’t. Spruijt et al recently reported on complex wounds which were receiving expert care by specialist wound practitioners in Europe. The wound aetiologies treated included diabetic ulcers, osteomyelitis, wounds in irradiated tissue, pressure injury and various leg ulcers. Healing rates were reported to be in the range of 44% to 71% after 4-6 months of treatment. Bringing challenging wounds to closure is prolonged, expensive and spiritually depleting for those who endure them. However the statistics above suggest that between 29% to 56% of complex wounds do in fact not heal. Non-healing wounds attract comparatively little commentary compared to literature which focuses on research, interventions and product. Yet these wounds are an horrendous lived experience. As clinicians we need to better prepare ourselves and our clientele for the “hard” discussions around non-healing and what clinical care should then look like. This is where patient centred care must be paramount.
Spruijt NE et al Stratification of chronic and complex wounds according to healing characteristics: a retrospective study. J Wound Care 2019;28(7):446-452.